NEW DELHI New Delhi: A recent study at Cedars-Sinai Cancer found that in 80 percent of cases, patients with early pancreatic cancer are misstaged.This finding highlights the critical need for improvements in staging and diagnostic techniques, which could have a substantial impact on early pancreatic cancer research and treatment.The study findings were published in the peer-reviewed journal JAMA.Researchers examined information on more than 48,000 patients in the National Cancer Database for this investigation.
Each patient in the study had either stage 1 or stage 2 pancreatic cancer, according to preoperative imaging. After surgery to remove the tumor, staging was increased in more than 78% of stage 1 patients and more than 29% of stage 2 patients — generally to a stage that included lymph node involvement. “Our research shows that staging — essential for making treatment decisions and determining resection eligibility — is often inaccurate in early-stage pancreatic cancer,” said Srinivas Gaddam, MD, associate director of Pancreatic Biliary Research at Cedars-Sinai and senior author of the study. “As the field continues to move toward earlier diagnosis, the importance of early staging will increase even more.”
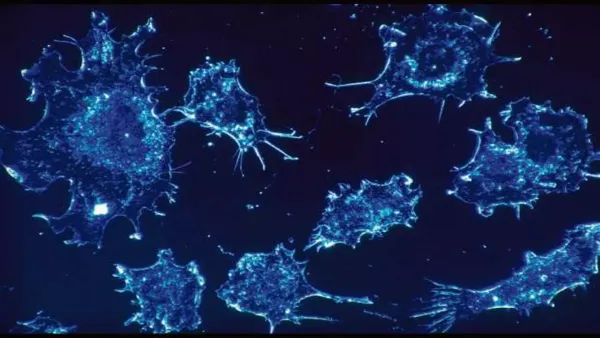
Diagnosing and staging pancreatic cancer is difficult for this reason. The pancreas, a digestive organ, is located deep in the body and current imaging techniques are not always able to detect small tumors or lymph node involvement, said Gaddam, who is also an associate professor of medicine and runs the Pancreatic Cancer Screening and Early Detection Program at Cedars-Sinai. Lymph nodes, groups of small immune structures, are an important factor in staging cancer and are a key differentiator between early-stage and later-stage pancreatic cancer. “Patients who have lymph node involvement have lower survival rates than those without lymph node involvement,” Gaddam said. “When imaging is unable to detect lymph node involvement, staging may not reflect the true extent of the disease. Our findings show that lymph node involvement is missed in four out of every five patients during the staging process.”
The five-year survival rate for stage 1 pancreatic cancer is greater than 83%, but this drops to just 3% for patients with stage 4 disease — which is where the majority of patients are currently diagnosed. “Pancreatic cancer is difficult to diagnose and there is a great need to improve outcomes for patients,” said Dan Theodorescu, MD, PhD, director of Cedars-Sinai Cancer and Distinguished Chairman of the Phase One Foundation.
“Through pioneering tools like our Molecular Twin Precision Oncology Platform, we are developing tests that will guide precision treatment of pancreatic and other cancers. We first demonstrated the utility of Molecular Twin by identifying new biomarkers for pancreatic cancer; these biomarkers aid in diagnosis, which should be combined with accurate cancer staging for appropriate treatment.”
Gaddam's message to physicians staging pancreatic cancer is to recognize the limitations of current imaging technology and to proactively assess and report lymph node involvement. And for those at the forefront of innovation, he emphasizes the urgent need to improve screening and diagnostic techniques.
MRI and endoscopic ultrasound are used to screen for pancreatic cancer. Screening is recommended for people with a family history of pancreatic cancer and for people who have variations in certain genes associated with the disease.
“We know that our current screening and staging tools are not good enough,” Gaddam said. “My hope is that within the next 10 years, we will develop advanced tools for screening and staging pancreatic cancer, allowing us to diagnose most patients at stage 1 and stage 2 rather than stage 4. With these advances, we can catch this disease much earlier, improving outcomes for many more patients.”